Which medical devices really need clinical data for initial CE-marking?
For which devices may data from the generic device group together with
advanced testing be enough for initial CE-marking?
Is advanced non-clinical testing better suited to support patient safety
than pre-market clinical data for some devices?
What do advanced non-clinical testing strategies look like?
What is the role of PMCF in this context?
Methods
Our methodology combines qualitative and consensus-building approaches.
Evidence Mapping
We categorize and assess both clinical and non-clinical data needs for different device types and risk classes.
Expert Interviews
We conduct in-depth interviews with stakeholders including clinicians, engineers, regulatory professionals, and device manufacturers.
Delphi Study
A three-round Delphi process engages experts across disciplines to build consensus on evidence requirements.
Timeline
Use Cases Round 1
Use Cases Round 2
Use Cases Round 3
Analysis
Delphi Round 1
Delphi Round 2
Delphi Round 3
Use Cases Round 1 – Well Established Technology
This phase focuses on implantable and class III devices, either listed under MDR 61(6b) or expected to be included in the update scheduled for Q3 2025.
Expert interviews will be conducted with medical experts in the respective fields.
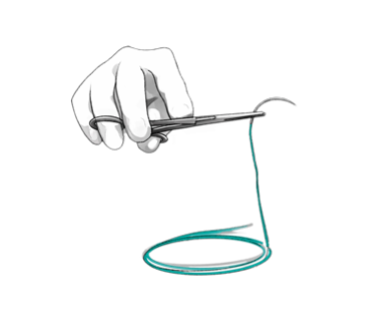
Suture
Classified as implantable, included in MDR 61(6b)
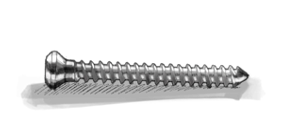
Bone Screw
Classified as implantable, included in MDR 61(6b)
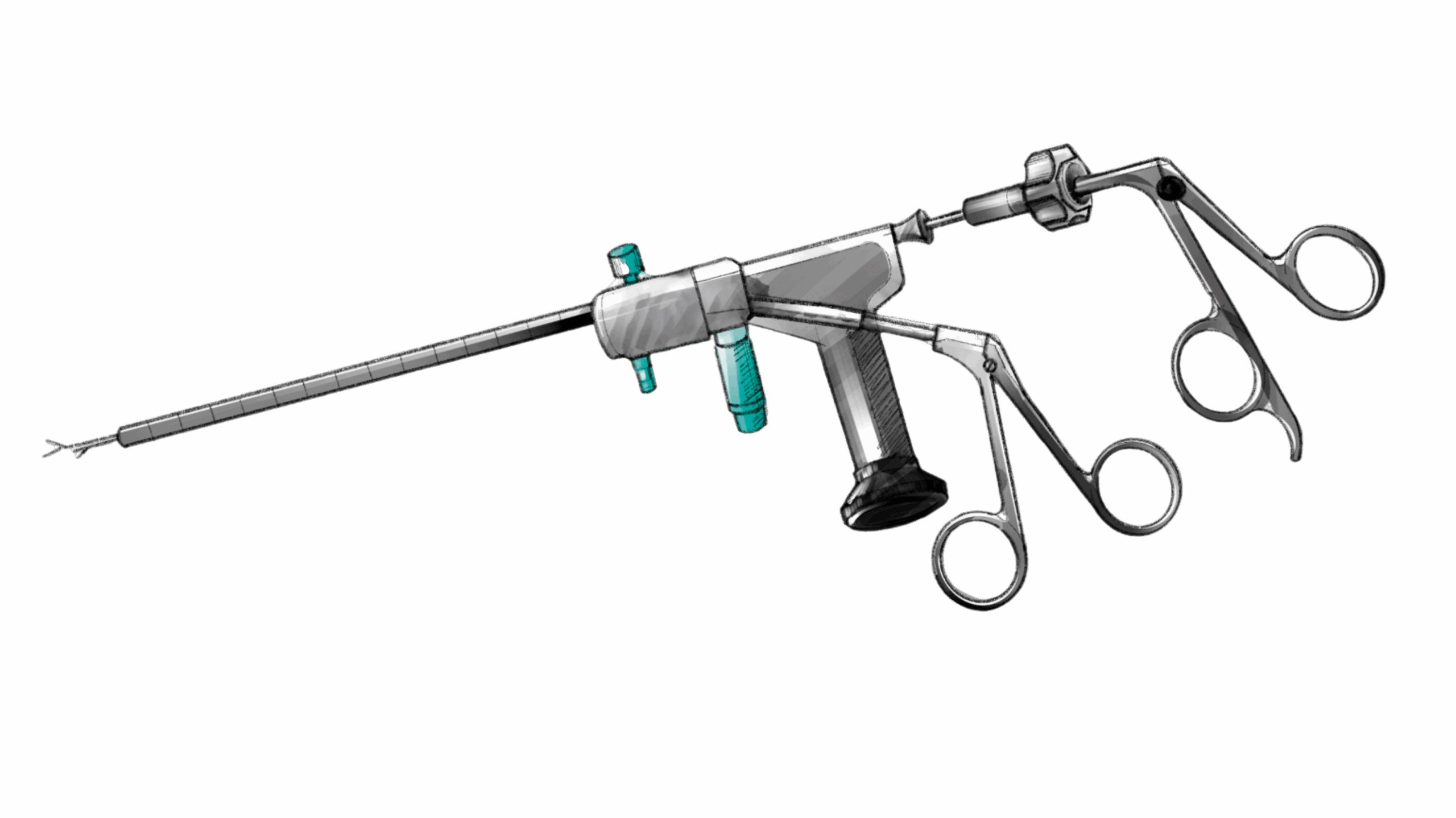
Instruments for Neurosurgery
Basic surgical instrument, class III due to contact with the central nervous system
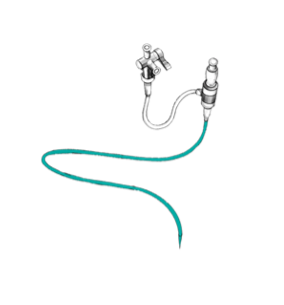
Introducer for Catheter/Stents
Simple design and no direct benefit, class III due to contact with the central circulatory system
Use Cases Round 2 – Active Medical Devices
The second round of use cases will focus on active medical devices. The primary emphasis of this phase will be on simulation and pre-clinical testing to validate interactions between the device and the human body in a non-clinical setting.
The following devices have been identified:
Additional devices will be included at a later stage.
Expert interviews will be conducted with medical and technical experts in the respective fields.
Team
This collaborative research is led by:
- Prof. Tom Melvin, University of Galway, Ireland
- Prof. Dr. med Michael D’Agosto, Hochschule Furtwangen University, Germany
- Elisabeth Oltmanns, Escentia GmbH, Germany